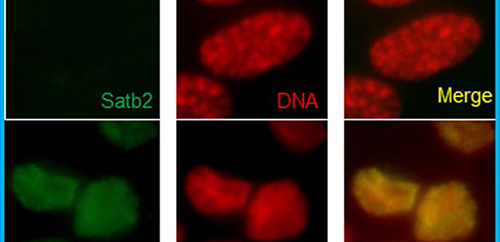
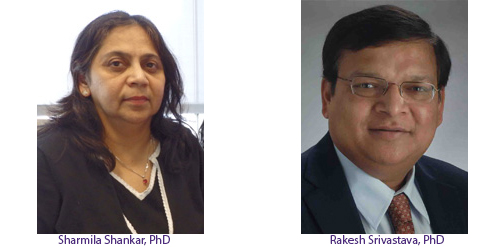
SATB2 is a novel “transcription factor” – a protein “switch” that controls which genes are turned on or off inside a cancer cell. Drs. Rakesh Srivastava and Sharmila Shankar identified it in the so-called “cancer stem cells” – cancer cells that behave like stem cells. Cancer stem cells are a small subset of immortal cells in tumors that are not only capable of renewing themselves, but also giving rise to other cells needed by the tumors to survive and grow. These cells are more resistant than typical cancer cells to standard chemotherapeutic agents and can persist in the body even after treatment. The cancer stem cells are thought to be a major cause of treatment failure, disease relapse and metastasis. Certain signals can turn a regular cancer cell into a cancer stem cell, making it resistant to treatment. SATB2 appears to be a master regulator of that process, controlling several of the mechanisms involved.
Silencing SATB2 in the colorectal cancer cells not only suppressed cell growth, motility and colony formation, but the characteristics of cancer stem cells were absent. This means that if agents are identified that can block SATB2, they may be used, along with standard of care, to prevent cancer relapses and metastasis.
According to the National Cancer Institute, colorectal cancer represents 8% of all new cancer cases in the US, with 135,430 new cases and 50,260 deaths expected this year. In 2014, there were an estimated 1,317,247 people living with colorectal cancer in the United States.
Other members of the research team include Drs. Wei Yu and Yiming Ma from Kansas City VA Medical Center.
The research on SABT2 was supported by a grant from the National Institutes of Health and a VA Merit Award to Dr. Shankar, who is also a senior scientist at the Southeast Louisiana Veterans Healthcare System.
The authors conclude that while their research suggests an oncogenic role of SATB2 in colorectal cancer initiation, progression and metastasis, future studies in transgenic mice are needed to confirm their results.