Medical Students Work on Health Policy on Capitol Hill

These students devoted the last summer vacation time they’ll have for a while to this program. “I really wanted to use my ‘last summer’ to learn about medicine from a completely different perspective that I would never get from the classroom,” said fellow Fellow Nicole Rueb.
“Medical students in the Health Policy Fellowship Program gain valuable experiences regarding the impact of policy on the delivery of health care,” said Peggy Honoré, MHA, DHA AmeriHealth Caritas-General Russel Honoré Endowed Professor at LSU Health New Orleans Schools of Public Health and Medicine. Dr. Honoré founded and leads the 4-year-old fellowship program made possible by the generosity of AmeriHealth Caritas Louisiana.
Thousands of Bills
Leslie Capo
Office: 504-568-4806
Cell: 504-452-9166
lcapo@lsuhsc.edu
Related
Health Policy Fellowship Application
Global Efforts to Combat Diseases
James Mickler, whose undergrad university was LSU, worked at the Centers for Disease Control and Prevention (CDC) Washington, D.C., office. He was assigned to the NCIRD (National Center for Immunizations and Respiratory Diseases) and NIOSH (National Institute for Occupational Safety and Health) accounts. He tackled such health issues as the measles outbreak on the U.S. and the resurgence of black lung disease in coal miners. But the highlight of his fellowship involved another serious health concern.


Surprise Medical Bills
Carley Boyce worked in Sen. Bill Cassidy's office. Two of her main assignments were the Surprise Medical Billing issue and Lowering Health Care Costs.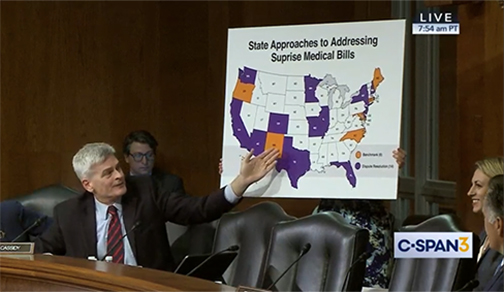
She helped create graphics for the senator to present supporting data. One was on the different health care costs by state.

Safety Net Health in Action
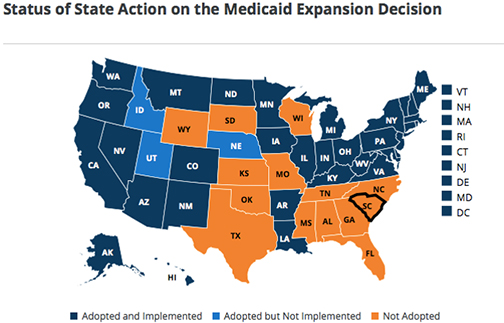
Baton Rouge native Caroline Bonaventure was assigned to the Association for Community Affiliated Plans (ACAP). ACAP is an association of 66 nonprofit and community-based Safety Net Health Plans located in 29 states. Collectively, ACAP health plans provide coverage to 20 million people enrolled in Medicaid, the Children’s Health Insurance Program (CHIP), Medicare Special Needs Plans and Qualified Health Plans.
She worked on a project to create a learning collaborative to push behavioral research to ACAP plans. Bonaventure’s role was to read, summarize and categorize 50+ behavioral health research projects funded by the Patient-Centered Outcomes Research Institute.

“It was so interesting to see the Congressional members at work and hear from the different witnesses, some of whom I recognized,” said Bonaventure.
“During these visits we got to learn more about health policy, the future of public health, and how to get involved as a physician in the future,” Bonaventure relayed.
On the Front Lines of Policy
Andre Florea was born in South Africa to Romanian parents and arrived in the U.S. at age 4. He was teamed with the National Academy for State Health Policy and researched why CHIP enrollment is falling in many states. He also worked on expansion of state-based health care exchanges.He feels the Fellowship program was the best thing he could have done in the summer following his first year of medical school.

Greater Access to Care
Nicole Rueb was matched with the National Rural Health Association (NHRA). She contributed to an analysis of rural hospital closures and how current policies affect rural hospitals. She also worked on access issues, specifically mental health, primary care and maternal health. Other areas included workforce shortages, important not only to access, but to the economies of rural areas because hospitals are often the first or second largest employer in a rural community.
“The fellows work on policy formulation and analysis tasks that provide them with real illustrations of how policy can influence improvements in the health of populations,” added Honoré. “These dynamic experiences help them understand how policy, as an essential service of public health, is a critical component to producing better health in the U.S.”
Dynamic Fellowship Shapes Future Practice
It was a seminal experience for these future doctors. One that really broadened their perspectives and horizons.
Added Florea, “Even though I plan to become a practicing physician, I will definitely incorporate public health policy and advocacy in my future career.”
Bonaventure gained new insight into health care. “This fellowship showed me how important it is for physicians to have a voice in health care policy and to advocate for patients and give firsthand insight into how policy shapes practice.”
Boyce expressed her gratitude to AmeriHealth Caritas, Dr. Honoré, Dean Nelson, and LSU Health New Orleans School of Medicine, “for giving me this unique and once in a lifetime opportunity! I’m so grateful for my incredible summer.”
Along with Honoré, three of this year’s fellows – Michael Bates, Caroline Bonaventure and Nicole Rueb – will present their newly gained expertise at the American Public Health Association annual meeting in Philadelphia in November.
And who knows where they’ll go from there.“Leadership skills gained through the fellowship experience prepare them for roles in advancing health system change,” explained Honoré.
Take Michael Bates. “The Health Policy Fellowship Program revealed a calling I have toward leadership in the health care sector of this country's political atmosphere.” But not for a while. “Prior to diving into health policy, I want to be a practicing physician for a long time after my residency training. To influence health care at the 30,000 foot level of Washington, D.C., before developing a ground-level understanding of patient care would be a disservice to patients and health care professionals equally. As a life-long goal, I would be honored to one day be considered for Secretary of the Department of Health and Human Services.”
