Study Finds New Single-Dose Antibiotic Safe and Effective for Uncomplicated Gonorrhea
A phase 2 clinical trial led by Stephanie N. Taylor, MD, Professor of Medicine and Microbiology in the Section of Infectious Diseases at LSU Health New Orleans School of Medicine, has found that a new antibiotic effectively treats uncomplicated urogenital and rectal gonorrhea infections in a single oral dose. Results are published in the November 8, 2018, issue of the New England Journal of Medicine.
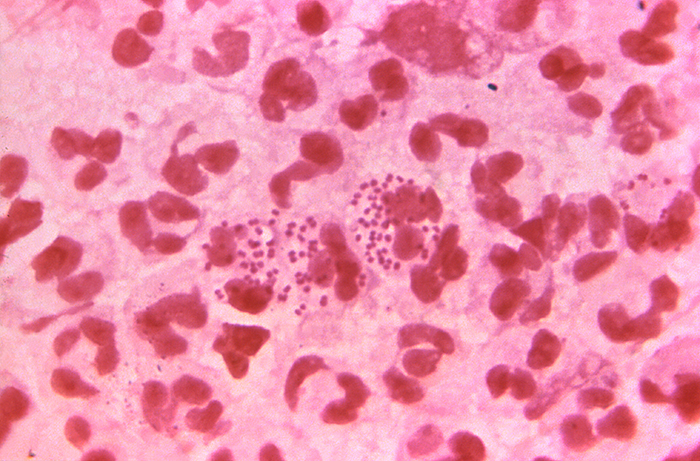
“According to the Centers for Disease Control and Prevention, the incidence of gonorrhea in the US increased by 67% from 2013 to 2017,” notes Dr. Taylor. “The bacteria causing gonorrhea, Neisseria gonorrhoeae, has developed resistance to every class of antibiotic currently recommended for treatment, and reports of multidrug-resistant N. gonorrhoeae necessitate the urgent development of new antimicrobial agents.”The researchers conducted a randomized, open-label phase 2 clinical trial to determine the safety and effectiveness of the investigational drug, zoliflodacin, in treating uncomplicated gonorrhea infections. Zoliflodacin, which has been fast-tracked by the FDA, works differently from the antibiotics currently available to treat gonorrhea. It inhibits DNA biosynthesis in a new way, impeding bacterial growth. Entasis Therapeutics in Waltham, MA developed zoliflodacin.
With a goal of 144 participants with gonorrhea, a total of 179 participants were enrolled at sexual health clinics in New Orleans, Seattle, Indianapolis, Birmingham and Durham, North Carolina from November 2014 through December 2015. The men and non-pregnant women, 18 - 55 years old, were eligible if they had signs and symptoms of urogenital gonorrhea, untreated urogenital gonorrhea or sexual contact in the preceding 14 days with a person who had gonorrhea. Urethral, cervical, pharyngeal and rectal swabs were taken at enrollment. Thirty-eight participants were excluded due to negative cultures. Participants were randomly assigned to receive a single, oral dose of either 2 or 3 grams of zoliflodacin or a single injected dose of 500 mg of ceftriaxone, one of the two drugs currently used to treat gonorrhea.The microbiologic intention-to-treat (micro-ITT) group (141 participants) included all participants with gonorrhea at urethral or cervical sites. The per-protocol group included the participants in the micro-ITT group who met all inclusion criteria, did not have another infection other than chlamydia or bacterial vaginosis, did not receive any other systemic antibiotic before test of cure and returned for a test-of-cure visit within a six-day window.
Treatment with 2 or 3 g of zoliflodacin resulted in a 96% cure rate in those with urogenital infections in the micro-ITT group, while the cure rate for those treated with ceftriaxone was 100%. In the per-protocol group, 98% of the participants who took the 2-gram dose of zoliflodacin and 100% of those who received the 3-gram dose, as well as all of the participants in the ceftriaxone group, were cured. All of those with rectal infections who were treated regardless of dose or medication were cured. Pharyngeal infections were cured in 4 of 8 participants (50%), 9 of 11 participants (82%), and 4 of 4 participants (100%) in the groups that received 2 g of zoliflodacin, 3 g of zoliflodacin, and ceftriaxone, respectively.
“Ceftriaxone is one of two drugs used as the current standard of care to treat uncomplicated gonorrhea,” adds Taylor. “A cephalosporin, it is the last class of antibiotics we have to treat gonorrhea. While it has worked well, we are starting to see resistance to it, too. Since there is no vaccine to prevent gonorrhea, and the possibility of untreatable gonorrhea is looming larger, it is imperative that we develop new drugs to treat it. Our promising early results suggest that zoliflodacin could be one of them.”
According to the CDC, gonorrhea is the second most commonly reported notifiable disease in the United States. In 2017, a total of 555,608 cases of gonorrhea were reported in the United States. Louisiana ranks second in the nation with 257 cases per 100,000 people reported last year. Infections due to Neisseria gonorrhoeae are a major cause of pelvic inflammatory disease (PID) in the United States. PID can lead to serious outcomes in women, such as tubal infertility, ectopic pregnancy, and chronic pelvic pain. In addition, epidemiologic and biologic studies provide evidence that gonococcal infections facilitate the transmission of HIV infection.Besides LSU Health New Orleans, participating centers include University of Alabama at Birmingham; University of Washington, Seattle; Indiana University, Indianapolis; and University of North Carolina, Chapel Hill.
The Division of Microbiology and Infectious Diseases (DMID) and the National Institute of Allergy and Infectious Diseases (NIAID) at the National Institutes of Health supported this research.